Table of Contents
What is Vitamin D?
Vitamin D is an essential nutrient that plays many vital roles in the body. Vitamin D is most well known for helping improve your body’s ability to absorb calcium and build strong bones. It also helps your body regulate calcium and phosphorus levels and helps support a healthy immune system.
This post may contain affiliate links through which we may earn a small commission to help keep this website free.
What does Vitamin D have to do with the kidneys?
The kidneys are known to play a very important role in Vitamin D use in the body. The Vitamin D that your skin creates and that is found in fortified foods and supplements is what we call “inactive Vitamin D”.
In order for organs in your body to use Vitamin D, it must be activated. In order for Vitamin D to be activated, it must first go to the liver where the liver will do the first step. The kidneys are the major organ to complete the second step to activate Vitamin D.
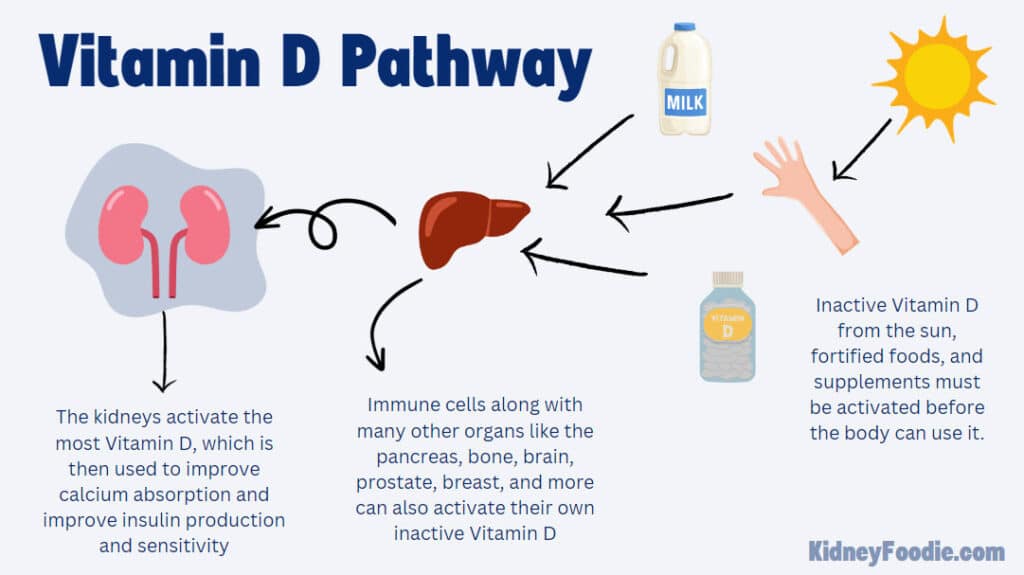
If you have Chronic Kidney Disease, your kidney’s ability to activate Vitamin D will go down. When the kidneys are not able to activate Vitamin D, the amount of active Vitamin D in your blood will go down.
Without active Vitamin D, some organs will not be able to get the Vitamin D that they need. For example, your intestines will not be able to absorb calcium as efficiently without adequate Vitamin D.
Inadequate calcium levels will in turn lead to bone breakdown and may increase your risk of osteoporosis.
Vitamin D also plays a role in anemia in CKD and can help to increase the number of red blood cells that are produced through stimulation of erythroid cells.
Is Vitamin D important for diabetes?
Vitamin D is known to play a role in insulin sensitivity and secretion of insulin. Infusion of active vitamin D into the blood of Vitamin D deficient kidney failure patients was found to both improve insulin sensitivity and improve insulin secretion.
Vitamin D is considered anti-inflammatory and may help reduce inflammation, which is common in people with diabetes as well as CKD.
People with diabetes are also considered to have compromised immune systems, and ensuring adequate Vitamin D status can help support a healthy immune system.
What are good sources of Vitamin D?
Vitamin D is not naturally found in high amounts in many foods. The major source of Vitamin D for many people is the sun. Your skin interacts with the sun’s rays to create Vitamin D.
Additionally, some foods such as milk are fortified with Vitamin D. Fatty fish such as salmon also contain Vitamin D, although people following a lower protein diet are unlikely to meet their Vitamin D needs from high protein foods like fatty fish.
Vitamin D Supplements for CKD
Many people rely on supplements to get their Vitamin D. There are two types of Vitamin D available over the counter: Cholecalciferol (also known as D3) and Ergocalciferol (also known as D2). Both supplements are considered effective for helping to maintain Vitamin D levels. If you are vegan and prefer only plant-based supplements, then you will want to look for ergocalciferol.
Some people take separate supplements for Vitamin D while other people may get their vitamin D through their renal vitamin or another supplement such as a calcium supplement. It is important to work with a dietitian to determine if your renal vitamin or other supplement contains an appropriate dose of Vitamin D.
Should you take Vitamin D if you have chronic kidney disease?
Determine your Vitamin D Status
If your Vitamin D levels are low, you may benefit from a supplement. A normal Vitamin D level is 30-100 nmol/mL. If your Vitamin D levels are below 30 nmol/mL, then you would be considered deficient. Your doctor or dietitian can help you determine an appropriate dose of Vitamin D to replenish your levels. Once your Vitamin D levels are within the normal range, they can help you determine an appropriate dose to take long term to maintain your Vitamin D levels.
It is recommended to check your Vitamin D levels at least once per year. We recommend checking levels in mid to late winter. Many people spend more time inside where they do not get exposure to the sun. If they do go outside, they are typically more bundled up with less skin exposed to the sun, so this is the time of year that you are most likely to see a deficiency.
Your skin’s ability to create Vitamin D from the sun goes down as you age, so the older you are, the more at risk you may be of having a deficiency. Additionally, the darker your skin tone, the more time you must spend in the sun to create your own Vitamin D. If you wear sunscreen, this will prevent your skin from being able to use the sun’s rays to create Vitamin D.
Do people with CKD need inactive Vitamin D?
It is important to note that the Vitamin D lab tests only for the inactive Vitamin D levels in your body. There is some confusion among healthcare providers on whether or not inactive Vitamin D levels matter for people with CKD, since the kidneys may not be able to activate it.
However, many of your body’s organs rely on inactive Vitamin D to perform their daily functions including the immune system, bone, prostate, colon, and pancreas (just to name a few!). For that reason, it is still important for people with CKD to maintain adequate inactive Vitamin D levels.
Both inactive and active Vitamin D will be important for people with kidney disease. Inactive Vitamin D is available as an over the counter supplement while the active form will need to be prescribed by your doctor based on your labs.
Is Vitamin D safe for people with CKD?
Over the counter Vitamin D supplements, when taken in appropriate doses are generally considered safe, however it is always important to talk with your doctor or dietitian before starting a new supplement.
There are some medical conditions where supplementing with Vitamin D may be inappropriate. In these medical conditions, parts of your body that normally do not activate a significant amount of calcium can start to activate large amounts of Vitamin D and lead to high calcium levels due to increased calcium absorption by your small intestines. Talk to your doctor before starting a new supplement to ensure that taking it is safe.


