In this article, we take a deep dive in potassium and how it relates to non-dialysis Chronic Kidney Disease. This article is for information purposes only, and not a substitute for medical advice or treatment. Always consult your doctor and healthcare team about your unique needs before making changes to your medications and diet.
This post may contain affiliate links through which we may earn a small commission to help keep this website free.
Table of Contents
What is potassium and how does it work in the body?
Potassium is a crucial but often misunderstood nutrient in the world of Chronic Kidney Disease (CKD). Gaining a clear understanding of its role in the body is vital for managing overall health.
The latin word for potassium is “kalium”, which is why the symbol for potassium is a “K”.
Potassium is an essential mineral in your body that plays a vital role in a lot of different processes. You may sometimes hear potassium referred to as an electrolyte. Some other electrolytes in your body include sodium, calcium, magnesium, and chloride.
These electrolytes carry an electrical charge, which is why they are called electrolytes.
Electrolytes are crucial for things like:
- Helping your nerves send messages so you can move, feel sensations, and think.
- Assisting your muscles in contracting and relaxing, allowing you to move and perform activities.
- Maintaining the right balance of fluids in your body, which is essential for your cells to function properly.
- Contribute to the regulation of your heartbeat and blood pressure.
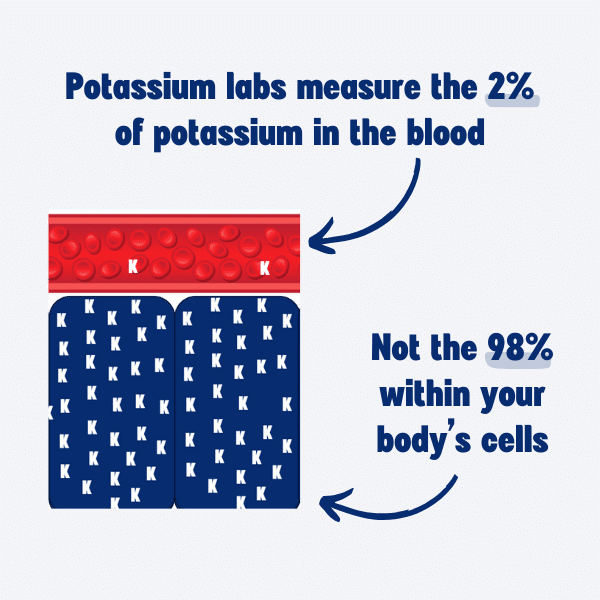
Potassium is located throughout your body. The majority of potassium – about 98% – is located INSIDE the cells of your body, so potassium is located inside things like your muscle cells, your brain cells, all the cells of your different organs, etc.
The rest of the potassium inside you – the other 2% – is located in the fluids of your body like your blood. It is important to maintain this balance of potassium between your blood and your cells, which is why your labwork typically includes a potassium lab to measure how much potassium is in your blood.
So how is potassium kept in balance in the body?
Many people assume that when you eat something that contains potassium- such as bananas- that the potassium goes into your bloodstream, and then your kidneys remove the extra potassium.
People also assume that if you have kidney disease and your kidneys don’t filter as well, then the potassium is just going to build up in your blood stream and cause your potassium levels to skyrocket.
That is not at all what happens though. What actually happens is that when you eat a meal (and that meal will almost certainly contain some amount of potassium), it not only contains potassium, but it also tends to have carbohydrates or proteins.
At the same time your body is absorbing the potassium from your meal, your body is also releasing the hormone insulin.
Most people who are familiar with insulin tend to think about it as a hormone that only helps with maintaining blood sugar levels, but it also plays a big role in maintaining potassium balance.
Insulin helps to signal to your body’s cells that you just ate a potassium rich meal and it tells the cells to pull some of the potassium out of the blood stream to help keep the blood levels in the right range. Our potassium levels stay in balance because insulin helped us remove the extra from the blood.
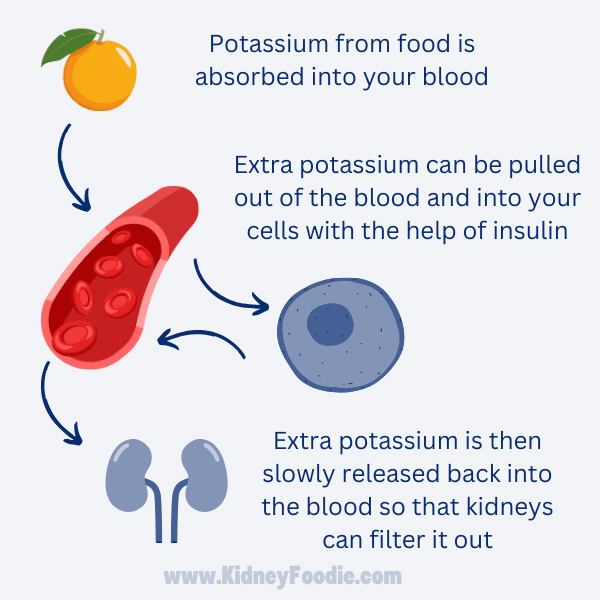
Later, when you’re not actively eating and absorbing more potassium, the cells of the body will slowly start to release that extra potassium that they took in during the meal digestion, and the kidneys will start to filter out any extra or unneeded potassium into your urine, so it can leave the body.
The kidneys can typically keep up with filtering out the extra potassium (assuming the cells are still doing their part by quickly pulling the extra out of the blood first) until the GFR gets to about 15. This is because the cells of the body are really slowly releasing the potassium from the cells, slow enough that even kidneys with reduced function can keep up. Many people with kidney disease don’t have any issues with handling potassium.
There are some circumstances that can cause this to get a bit imbalanced, but the big takeaway from this article is that what you eat doesn’t always impact your potassium levels the way you think it would.
When we talk about managing potassium levels, we are pretty much always referring to the blood levels of potassium. 98% of potassium in the body is found inside your cells, so when we talk about managing potassium levels, we are really talking about that other 2% of potassium that is found in the blood serum.
A normal potassium level is 3.5-5.0 mEq/L or it is sometimes also listed as mmol/L.
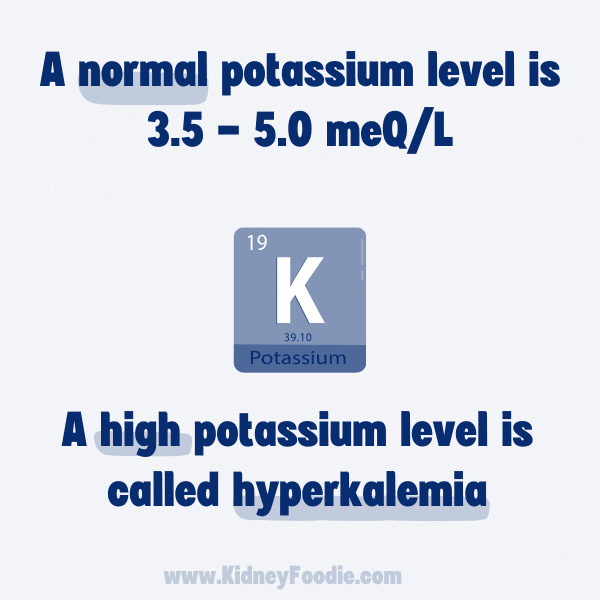
If your potassium level is less than 3.5, then that is called hypokalemia. If your potassium levels are higher than 5.0, then you have hyperkalemia.
Both low and high potassium levels pose risks, manifesting in symptoms like muscle weakness and cardiac problems. While slow increases are generally tolerated, serious consequences arise with rapid or significantly elevated levels.
It is important to determine the cause of out-of-range potassium levels to develop the right strategy for correcting it.
Things that can affect your potassium lab draw
In kidney disease, especially chronic kidney disease, high potassium levels (also known as hyperkalemia) are the more common problem when someone has potassium out of range. It is often assumed that high potassium levels are caused by eating too much potassium from high potassium fruits and vegetables, but this is not usually the cause of high potassium levels – even in kidney disease.
In some cases, there are a few things that you might be doing before lab draws to cause your potassium levels to be higher than they should be.
And when I say “higher than it should be”, I’m referring to something called pseudohyperkalemia. Pseudohyperkalemia occurs when you have a high potassium lab value, but your actual potassium levels are not high.
Fist Clenching and High Potassium Levels
One of the more common ways that people can cause their potassium lab values to be falsely high is through fist clenching.
Frequently when you get blood drawn, the person drawing the blood may put a tourniquet around your arm to make the blood vessels more prominent. At some point in your life, you may have also been given a ball to squeeze or been asked to make a fist to help make sure your veins are easy to find. But what researchers and healthcare providers have found is that this technique of clenching your fist can actually cause your potassium levels to be temporarily high.
Clenching your fist activates the muscles in your arm and when your muscles are activated, they will temporarily release potassium into the blood. And remember, there is a lot of potassium in the cells of your body, so when they start to release potassium, it can make a big impact on your potassium levels. And then when you combine that with the tourniquet around your arm which prevents all that potassium from spreading out, the blood in your veins can actually become quite concentrated in potassium.
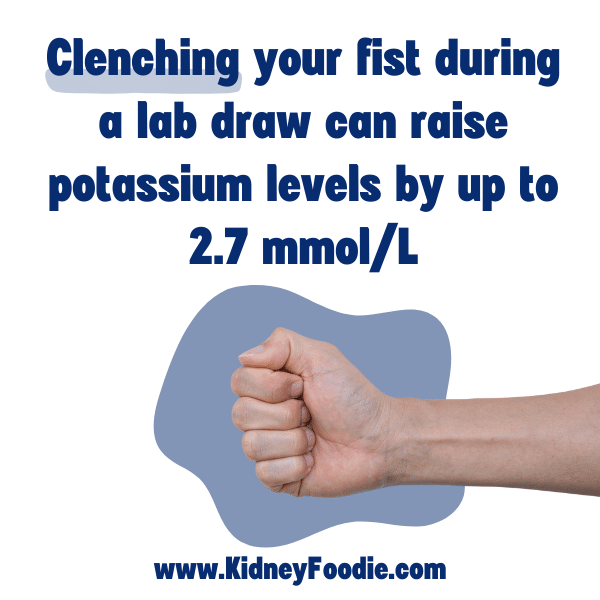
They have done studies on this and we know that this can actually raise your potassium levels by a substantial amount. Your actual potassium level could be 4.5 which is normal, but fist clenching caused it to be 5.5 – which is considered high.
There were even some individuals in these studies whose potassium’s went up by 2.7 mmol/L. That is a HUGE increase. You wouldn’t have any other signs or symptoms of something that would cause high potassium levels, so this could result in you being told to limit your potassium intake via food, when you really don’t need to be doing that.
Now, I will admit that the study participants who had the really big increases were the ones who were squeezing the hardest, but the researchers did make a point of saying that even really minor squeezes, like just barely flicking your fingers a couple of times made people’s potassium levels go up by .5 mmol/liter, which could be a meaningful amount.
So the next time you get your lab work done, double check that you aren’t instinctively clenching your fist in an effort to help make your veins easier to find. The tourniquet is fine. It is the muscle movement that causes the potassium to go up.
If for some reason, the technician drawing blood doesn’t think they can get a good needle stick without doing some fist clenching, then an alternate option to avoid the false high potassium levels is to make sure that they draw your potassium lab last.
For better or for worse when we get lab work done, they normally have to draw several tubes worth of samples to run all of the different tests. If you have to clench your first, then be sure to stop clenching as soon as they have inserted the needle.
If the tourniquet is removed and a couple of samples are drawn first, the chances of the last sample being high in potassium are substantially lower. There will have been adequate time for the potassium released from the arm muscles to disperse and return to your true potassium levels, which is what we really want to see when we are drawing a potassium lab.
Exercise
Along the same lines as fist clenching, exercise can cause temporary increase in potassium levels because of potassium being released from the cells of your body. Exercise is great for you and there are SO many reasons to exercise (so I am absolutely not telling you to avoid exercise if you have high potassium levels or are concerned about high potassium levels!).
However, you should avoid intense exercise right before your labs are drawn, which is usually not a problem for most people. This would cause an artificial rise in your potassium lab, and we wouldn’t want to be making decisions about what you should or shouldn’t be eating because of a normal, temporary shift in potassium from the exercise.
Low calorie beverages on an empty stomach
The last thing I see people do that can cause their potassium to be a bit high during lab draw (even if their potassium is otherwise normal the rest of the day!) is that they didn’t eat and they drank something high in potassium, but low calories.
When you eat a food that contains potassium such as a banana, it typically also contains carbs or protein. The carbs and protein will stimulate your body to release insulin, and insulin helps the cells of your body absorb potassium from your blood and keep things in balance.
If you eat or drink something that has potassium but very little carbs or protein like black coffee , this will not stimulate any insulin release, and then potassium can build up and result in high potassium levels.
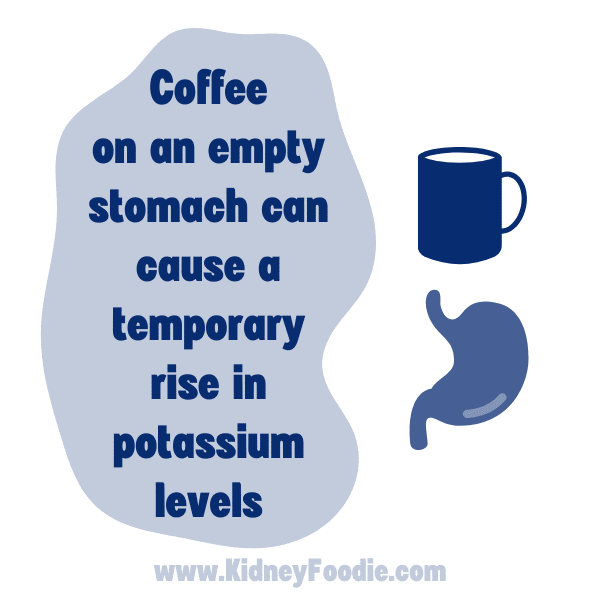
A common way I see this happen is in people who don’t eat before appointments. Perhaps they are fasting or simply don’t like breakfast, or just didn’t have time. BUT they are drinking beverages that contain potassium.
Examples of this would be black coffee, or unsweetened coffee as well as unsweetened tea. Coffee and tea are very popular beverages, and they both contain some potassium. Coffee has a bit more than tea.
Neither of these drinks are particularly high in potassium, but because these beverages are naturally very low in calories, they won’t stimulate your body to release more insulin. That means the cells of your body aren’t going to be equipped to remove some of the extra potassium until you decide to eat something later that stimulates insulin release.
If you’re getting your labs done, I don’t recommend drinking a lot of coffee or tea beforehand unless it is with your breakfast so you can get a more accurate picture of your potassium levels. Again, we don’t want to make decisions about what kinds of foods we can or can’t eat because of a potassium lab that wasn’t really a true reflection of our potassium status. That same lab taken at a different point in the day when you’ve eaten a meal would likely be lower than it is after drinking just black coffee all morning.
Along these same lines, if you have type 1 diabetes or are insulin dependent with type 2 diabetes, then you want to be sure that you are always taking your insulin as prescribed. If you miss a dose before a lab draw, you may see our potassium levels go up because your body can’t balance potassium well without adequate insulin.
By getting an accurate potassium lab, we can make more informed decisions about how to manage our potassium without being overly restrictive with the foods we eat.
Constipation and Potassium Levels in CKD
Constipation is a VERY important and common cause of high potassium levels in people with kidney disease.
For the vast majority of people, when there is extra potassium in your body, that extra potassium is filtered out by your kidneys. In people with healthy kidneys, about 90% of excess potassium leaves the body in the urine. The other 10% leaves the body in the stool, or your poop.
An interesting thing about kidney disease is that as kidney disease progresses and the kidneys are less able to filter out potassium in urine, the amount of potassium that leaves the body through the stool, or your poop, actually starts to increase.
As much as 75% of daily potassium intake could leave the body through your poop, which is A LOT of potassium. There is a catch though.
In order for your body to effectively eliminate potassium through your poop, you can’t be constipated.
If you’re not pooping, then obviously you aren’t getting rid of any potassium in your poop. But even when you do have a bowel movement while constipated, there won’t be much potassium in it if your stool is hard, and dry. The softer your poop is, the more potassium is being removed from your body.
Looking at a Bristol stool chart, like the one pictured below, can be a great way to see if you have the ideal poop for managing potassium levels. When you’re constipated, you’ll typically have stool or poop that looks like Type 1 or 2. It’s hard, lumpy, possibly in small separate lumps, and it can be difficult to pass. This is not ideal.

You really want to shoot for poop that is closer to type 4. You want your bowel movements to be smooth, soft, and shaped like a sausage or snake. Again, the softer your poop, the better.
If your poop is already a type 4, great. Keep up the good work. If it’s not, then what can we do to make it better?
One of the best ways that you can improve the type of poop that you have is by making sure that you get adequate fiber in your diet.
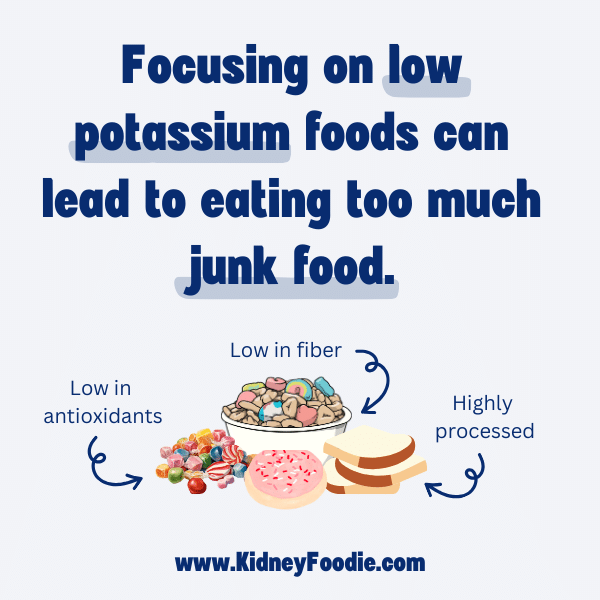
In my experience working with people with CKD, a mistake that people often make is to start focusing their diet on low potassium foods. In doing so, they tend to gravitate towards highly processed foods that have no fiber.
When your diet is low in fiber, you’ll get constipated and this WILL impact your potassium levels. When this happens, I sometimes see people double down on limiting potassium and it just compounds the issue because they make their constipation worse.
As an example, if you compare white rice to brown rice, you can see that white rice has 0.4g of fiber per 1 cup serving and about 35mg of potassium while brown rice has 3.2g of fiber per serving but 174mg of potassium.
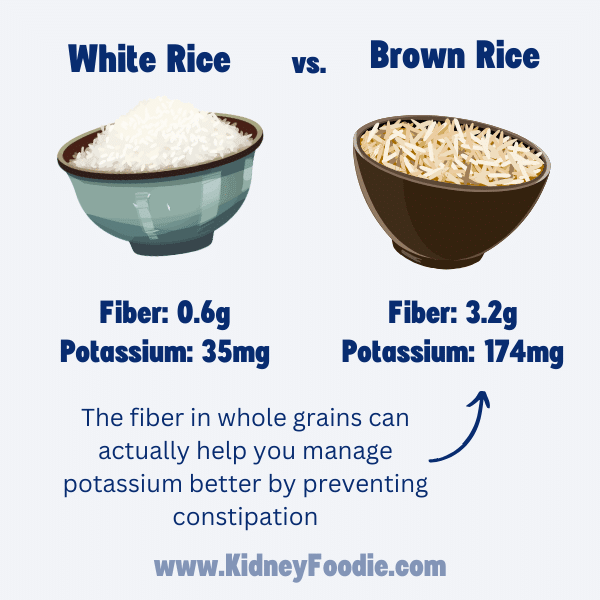
Some people look at that nutrition information and pick the lower potassium food thinking it is better for their kidney disease, but that is not actually the case. The brown rice is probably the better pick for most people because of the higher fiber content.
Some people also mistakenly believe that whole grains are high in phosphorus, but whole grains are not considered high potassium foods or high phosphorus foods and are a great option for people with kidney disease.
The recommended amount of fiber to get into your day is 14g of fiber for every 1000 calories you eat. If you eat 2000 calories a day, you would want to get in at least 28g of fiber. If you eat 3000 calories a day, then you should aim for 42g of fiber per day. It is fine to get more than that, especially if it is coming naturally from the foods that you are eating.

Foods that are naturally high in fiber include fruits and vegetables, which are especially good for people with kidney disease despite being higher in potassium than some other foods. Beans, whole grains, nuts, and seeds are also high in fiber. These can all be great choices for people with kidney disease who are trying to get in more fiber.
Where you get your fiber does matter. I don’t typically recommend fiber supplements in people with kidney disease, especially if you are on a fluid restriction because fiber supplements can actually make you more constipated if you don’t drink enough water with them.
I highly recommend getting fiber from natural sources. Foods that are naturally high in fiber also tend to be high in vitamins, antioxidants, and nutrients that are great for your kidneys and other organs, so there are multiple benefits to obtaining fiber from natural sources.
If you are concerned about your potassium levels, or you are having issues with high potassium levels, then start paying attention to your bowel movements. It is very important for people with kidney disease to have regular, easy to pass bowel movements to help maintain their potassium balance.
The best way to accomplish this is through a diet that is high in high fiber from unprocessed foods like fruits and vegetables, beans, whole grains, nuts and seeds.
If after modifying your diet to get adequate fiber, you are still having issues with constipation, talk with your doctor about other options to manage constipation or if there may be other underlying issues causing constipation.
How Metabolic Acidosis Affects Your Potassium Levels
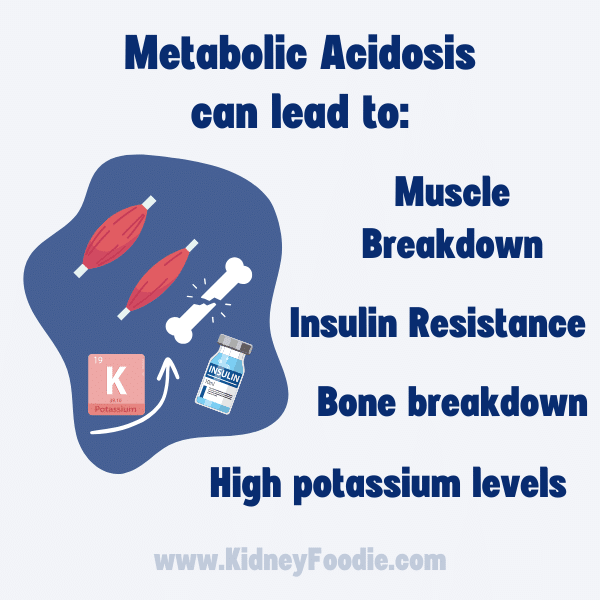
Metabolic acidosis is one of several things that can cause a person with CKD to be more prone to high potassium levels.
Metabolic acidosis is a condition in which there is too much acid in your blood and other fluids or tissues in your body.
Intuitively, we all know that having too much acid anywhere is probably not a good thing. Acid will cause damage. The body does not want your blood to be acidic, so your body will try to correct this.
In people with healthy kidneys, the kidneys actually help a lot to neutralize acid and remove it from the body.
When your kidneys are impaired, like they are with chronic kidney disease, then the kidneys may not be able to completely correct metabolic acidosis, so the body will try to compensate for this in other ways.
One of the ways it does this is by having the cells of your body pull acid out of the blood. While this sounds great at first, there is a catch. When your cells pull the acid out, they are exchanging it with potassium.
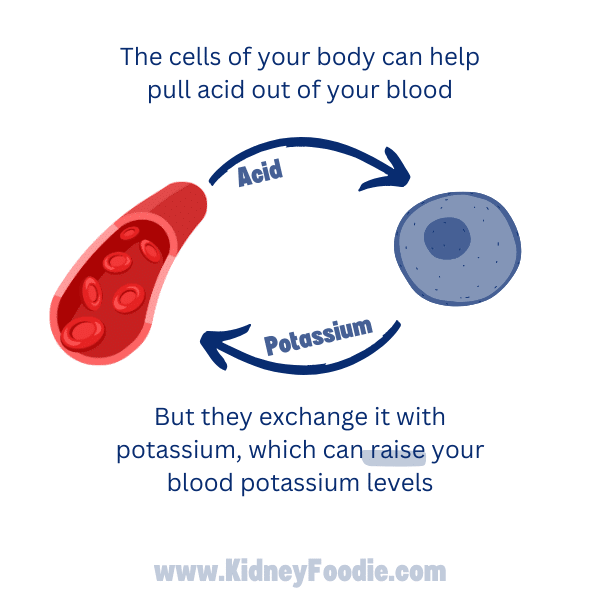
Your cells will pull acid out of the blood, but they will put more potassium into your blood in exchange. Given that 98% of the potassium in your body is inside your cells, there is a lot of potential potassium that they can exchange and this can really drive up potassium levels.
In addition to high potassium levels, acidic blood can also lead to more muscle breakdown, bone breakdown, as well as insulin resistance (just to name a few!). Controlling metabolic acidosis is not only going to be important for your potassium control, but it can also help keep your muscles and bones healthy.
To check and see if metabolic acidosis is possibly something contributing to your potassium issues, you can check your labs. You’ll want to look for a lab called CO2, carbon dioxide, serum bicarbonate, or bicarbonate – it can go by a lot of names.
For people with chronic kidney disease, the KDOQI nutrition guidelines suggest focusing on a target level of 24 -26 mEq/L. this is an interesting lab test because the normal range that is normally listed by lab companies can be as low as 20-21 mEq/L, so it’s not always going to jump out at you that your lab result is low.
If your levels are less than 24, then your blood is more acidic and metabolic acidosis could be contributing to high potassium levels. In this case, the best way to prevent the potassium issues is to prevent or treat the metabolic acidosis.
There are a number of things that could be causing metabolic acidosis, but one of the biggest things (and it’s one that most people can control) is what you eat.
When we eat food, it gets broken down in our bodies to provide nutrients to our body, but this breakdown creates some byproducts.
It’s kind of like when you burn wood in a fire. The burning wood is going to generate some good things, like heat to keep you warm, but it’s also going to generate some stuff you don’t want, like a big pile of dirty ashes when it’s done.
A similar thing happens with some foods that you eat. Your body uses the food to do all kinds of good things in your body like give you energy, but the process of generating that energy can leave some not-so-nice byproducts like acid in our blood.
Certain foods generate more acid than others. The biggest culprits are animal proteins such as meat, fish, or poultry as well as some dairy such as cheese. These foods are higher in compounds that will turn into acid inside your body.
One strategy to help reduce your metabolic acidosis is to reduce your consumption of these types of animal products. Since most CKD diets are somewhat limited in protein, you may find that you are eating less of these foods already.
There are also foods that help to neutralize acid. So another strategy that you can take to help reduce metabolic acidosis is to start including more foods that help to neutralize acid.
The best foods to eat to neutralize acid are going to be fruits and vegetables, particularly vegetables. It is interesting that a problem like metabolic acidosis can contribute to high potassium levels and that a potential treatment for metabolic acidosis is to eat more foods that are typically higher in potassium.
However, this just helps to illustrate that high potassium levels are frequently not caused by eating too much potassium. In the case of metabolic acidosis, the cause is potassium shifting out of your cells. It is really important for people with CKD to eat adequate fruits and vegetables.
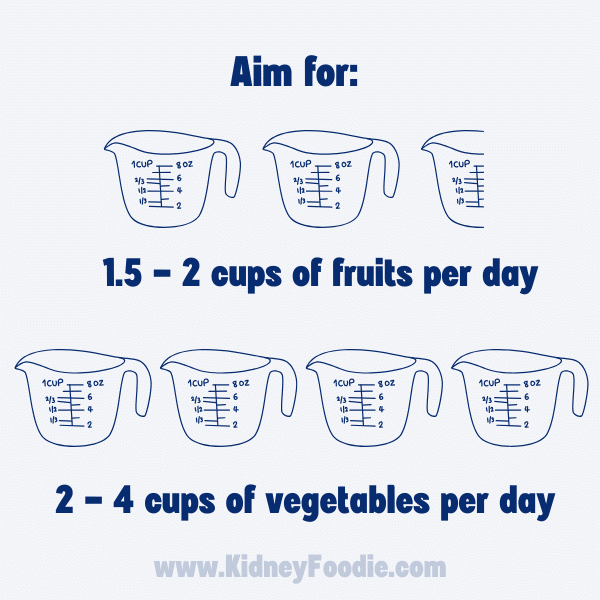
The Dietary Guidelines for Americans recommend that adults should aim for 1.5-2.5 cups of fruits per day and 2-4 cups of vegetables per day, which is something that people with CKD should strive for as well.
Your doctor may also prescribe a medication called sodium bicarbonate. This medication can also help to neutralize acid, although it is not a substitute for eating adequate fruits and vegetables because isn’t going to have all of the other benefits of fruits and vegetables.
If you are struggling with metabolic acidosis, despite making dietary changes to lower your intake of animal protein and increase your intake of fruits and vegetables, then taking this medication may be a good next step.
In summary, if you are having issues with controlling your potassium levels, be sure to rule out metabolic acidosis as a cause of your high potassium levels. Making changes to your diet to prevent metabolic acidosis like decreasing your intake of animal based proteins and getting in adequate fruits and vegetables may be beneficial.
It can seem paradoxical to eat more fruits and vegetables when you may be having some issues with your potassium levels, but controlling your metabolic acidosis can have a really big impact on your body’s ability to manage potassium levels.
The potassium found in food is not that high compared to the potassium that is being stored in your cells. If your high potassium levels are being caused by a shift in potassium out of your cells, then the most effective way to fix the high potassium level is to fix what is causing that shift, NOT to limit our intake fruits and vegetables. In the case of acidosis, that may just make the problem worse.
Salt substitutes and ultra high potassium foods
Potassium intake from foods is not usually the primary cause of a high potassium levels in people with CKD, but in the case of salt substitutes and potassium additives, the amount of potassium being ingested can really add up.
People with kidney disease are often told to cut back on their sodium intake. Something that is often advertised to people trying to follow a low sodium diet are what we call salt substitutes, which I have pictured below.

Salt substitutes are made of potassium chloride. One teaspoon of salt substitute contains 2,760mg of potassium, which is a LOT of potassium, especially if you add that on top of all the other things in your daily diet that contain potassium.
For anyone who is trying to avoid high potassium levels, we generally recommend avoiding these salt substitutes. If you’re trying to cut back on your sodium intake, but still want flavor, it is typically recommended to try different spices and seasonings rather than a salt substitute.
If you struggle with low potassium levels, your dietitian might actually recommend using salt substitutes, but this would only be if you have low potassium levels and should only be used at the recommendation of your healthcare provider. Otherwise, you should avoid these.
If you don’t use a salt substitute, you may be inadvertently eating foods that contain a lot of potassium chloride, or perhaps another potassium containing additive. Sometimes these foods can have A LOT of potassium in them.
Let’s look at some examples and talk about how to spot these ultra high potassium foods.
First up, soup. Soup can be a problematic food for people with kidney disease. Soup is often LOADED with sodium – crazy amounts of sodium. Like you could get your whole day’s worth of sodium just from a bowl of soup. It’s wild. And the soup manufacturers know that, and so they come up with these reduced sodium and low sodium versions of their soups to make you think that these are healthier. Here is an example:
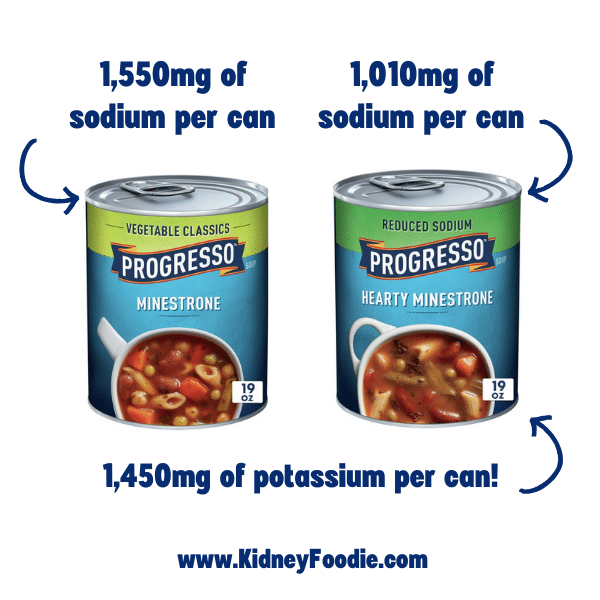
This can of Progresso minestrone contains about 1,550mg of sodium, and they also make a reduced sodium version of minestrone. The reduced sodium version contains 1,010mg of sodium, which is still A LOT of sodium. The way they were about to reduce the sodium without the soup tasting terrible is they replace it with potassium chloride.

As you can see in the ingredient list and nutrition fact for the reduced sodium soup above, it lists out potassium chloride as an ingredient.
Anytime you see a food that is “reduced sodium” or “low sodium”, you should check and see how much potassium is in the food because often times they are using salt substitutes to help reduce the sodium but still give the food a salty flavor, which ends up adding a lot of potassium to foods.
This ONE CAN of reduced sodium soup contains 1,450mg of potassium. That’s almost 3.5 bananas worth of potassium. And, interestingly, their regular minestrone also contains potassium chloride, so it’s not just the reduced sodium versions that will contain it.
Let’s look at another reduced sodium product. Let’s compare regular V8 and reduced sodium v8.
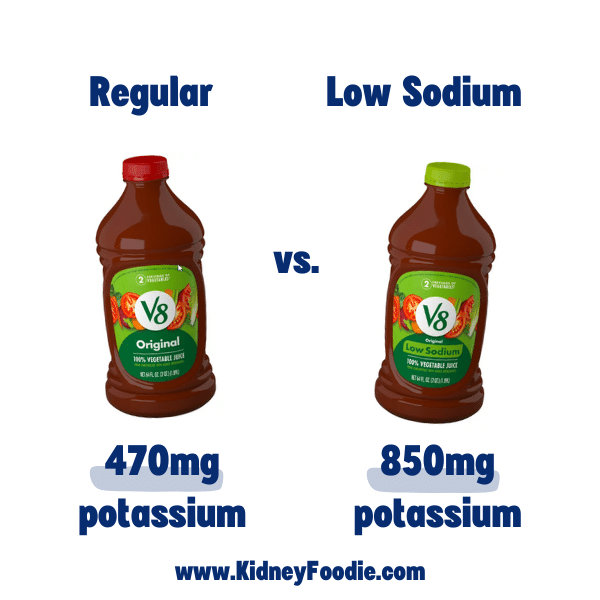
Regular v8 has 470mg of potassium per serving, which is not a small amount of potassium (which is to be expected with a concentrated tomato product like this). However, compare that to the low sodium v8, which has a whopping 850mg of potassium. All of that additional potassium is likely coming from the salt substitute potassium additive.
Definitely be sure to check labels carefully when shopping, especially if you tend to gravitate towards lower sodium foods.
Let’s look at another example that isn’t necessarily claiming to be reduced sodium. Let’s look at this lean cuisine herb roasted chicken. This little frozen meal contains 960mg of potassium.
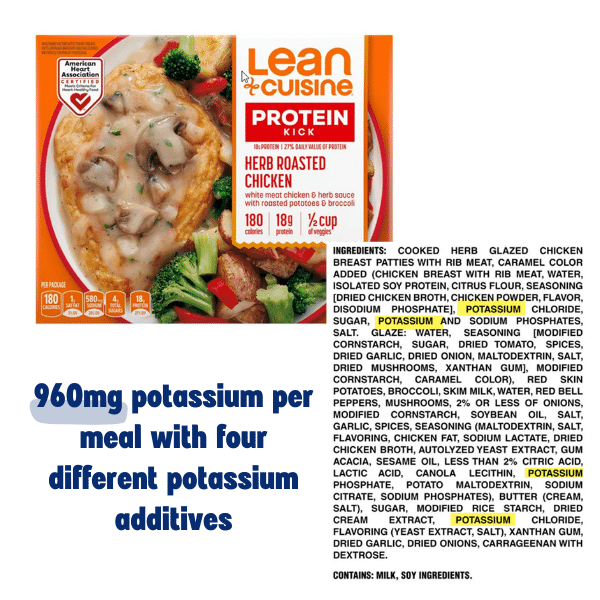
Based on how much potassium is typically found in foods like chicken and potatoes, I would estimate that approximately 200mg of potassium are coming from the chicken and up to 294mg are coming from potatoes and other vegetables. This means that roughly 460mg in the meal are coming from some other source.
If you review the ingredient list, you can see that potassium is listed a few different times. So I’m guessing that the remaining 460mg of potassium is coming from these additives. Essentially, a large banana’s worth of potassium has been added to this meal without anyone really realizing it.
Now, one thing I want to point out is the chicken here. You can see that the chicken has a whole lot more than just chicken in it. In addition to a lot of other stuff, you can see that it includes both potassium and phosphorus additives.
Potassium and phosphorus additives are VERY common in meat products. We usually call these “enhanced” meats. The additives are put in there to enhance the flavor and juicy-ness of the meat, and they can REALLY add up. Depending on how much is added, they can easily double or triple the amount of potassium in meat.
Now, there is a problem with figuring out how much potassium is in enhanced meats. With all of the examples I’ve done so far, we could look at the food label and see exactly how much potassium was in the food. With meat products, they aren’t required to put potassium on the labels. When manufacturers aren’t required to put something on a label, they usually don’t.
Let me show you an example of these ham cubes.
These ham cubes definitely contain added potassium, as you can see here on the ingredient list….but looking at the nutrition facts, you’ll have no idea how much, because it isn’t listed. And it can be really tempting to assume that if it isn’t listed, then it must be zero, but that could NOT be further from the truth.
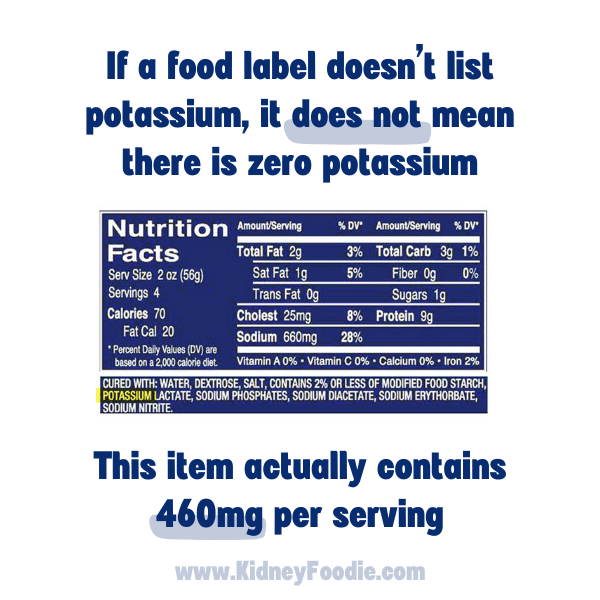
Now, for this particular example, I was able to find an entry in the USDA food database, where they did at one point report the potassium content of these ham cubes. And according to that, each 2 ounce serving has 460mg of potassium. A typical 2oz serving of cooked pork should only have about 200mg of potassium in it, so they added quite a bit of potassium to this product. And this is not uncommon. Enhanced meats tend to contain a lot of potassium.
If you’re struggling with potassium, avoid salt substitutes that contain potassium chloride and check foods labels for added potassium as this can be a big source of potassium in the diet, especially for people trying to follow a low sodium diet.
Always check to see how much potassium is listed on the label to see if it is a lot, and if it isn’t listed, then you definitely need to be scanning that ingredient list for potassium additives – especially in the case of enhanced meats. If it contains an additive but doesn’t tell you the amount, then just assume that it is going to be a lot.
Medications and supplements that affect potassium levels in CKD
Certain medications and supplements can affect your potassium levels.
Supplements that affect potassium levels
There are a lot of supplements on the market that contain potassium, and some can contain quite a bit of potassium, so they can have a big impact on your potassium levels.
People buy potassium supplements for a variety of reasons. Maybe they read somewhere that more potassium can help with their blood pressure. Maybe they read somewhere that taking potassium after a workout can help with muscle recovery.
Regardless of the reason, I highly recommend that you take a close look at the supplements you are taking to make sure that they don’t contain a high amount of potassium. Even people who have no kidney problems can end up taking life threatening amounts of potassium through supplements, so if you have issues with high potassium levels, review what supplements you are taking.
One of the sneakiest ways I see people getting in too much potassium is through electrolyte drinks, so if you’re drinking any electrolyte drinks, then those are going to have a decent amount of potassium.
Even if your supplement doesn’t seem to have a ton of potassium, keep in mind that many of these pills or drinks contain zero calories. If something doesn’t have any calories, then it isn’t going to stimulate your body to release insulin, and insulin is a major regulator of potassium in the body.
Insulin helps to remove extra potassium from your blood and store it safely inside your cells. Even if your supplement contains only 100 or 200mg of potassium, it can have a much bigger impact on your blood levels of potassium than the same amount of potassium from food would.
Medications that affect potassium levels
In addition to supplements, there are also some medications that can contribute to potassium problems, especially in people with CKD.
Non-steroidal anti-inflammatory drugs (also called NSAIDs) can affect the kidney’s ability to remove potassium from the blood and cause high potassium levels, especially in people who have kidney problems. Even just two days of taking an NSAID can result in life threatening hyperkalemia.
NSAIDs can have a number of negative impacts on kidneys (not just on how they handle potassium), so it is often recommended to discontinue using NSAIDs if you have kidney disease.
Ibuprofen, naproxen, and aspirin are common over the counter NSAIDs, but there are also prescription NSAIDS. Whatever you are using NSAIDs for, you should talk to your doctor about an alternative option.
A really good practice to get into with your healthcare providers is either keeping a comprehensive list of every medication and supplement you are taking, or just putting them all into a bag to bring to appointments periodically so that your healthcare team knows about everything that you are using.

More often than not, people are inadvertently taking something they no longer need, or have conflicting medications, or are taking something that is causing a problem that no one realizes. Always let your healthcare team know about all supplements and medications that you take so they can provide the best care possible for you.
There are also some prescription medications that can affect the way your body handles potassium. The most common ones seen in people with CKD are blood pressure medications such as ACE inhibitors and angiotensin receptor blockers.
Ace inhibitors are the medications that end in “pril” such as lisinipril while angiotensin receptor blockers, or ARBs for short, end in “artan” like losartan. Both of these types of medications have strong benefits in people with kidney disease and high blood pressure, so they are recommended medications, but they can predispose you to higher potassium levels.
If your GFR is higher than 40, the risk of hyperkalemia or high potassium levels is lower, so being on one of these medications does not guarantee that you’ll have high potassium levels.
Additionally, there are certain types of diuretics that can cause higher potassium levels while there are other types of diuretics that can result in lower potassium levels. Combining an ACE inhibitor or ARB with a diuretic that helps reduce potassium levels can balance out the effects on potassium levels, so some people see no changes in their potassium levels when taking these medications.
ACE inhibitors and ARBs are really beneficial medications for people with kidney disease, especially if you have high blood pressure, so I encourage you to continue taking these medications as prescribed by a doctor, despite the possible risk of increasing potassium levels.
If you do have issues with potassium on these medications, addressing other potential causes of potassium, such as constipation, insulin issues, metabolic acidosis, use of NSAIDs, etc can offset the effects of these blood pressure medication.
If you are having problems with your potassium levels while taking an ACE inhibitor or ARB, you should explore other contributing factors to the high potassium before assuming that you need to drastically cut back on your potassium intake.
So just to summarize, supplements and medications CAN have an impact on your potassium levels. Check all of your supplements and verify that they don’t contain any potassium.
Keep a detailed list of all supplements and medications that you take that you can share with healthcare providers to help them get a full picture of your health and whether any supplements or medications could be doing more harm than good.
Last, but not least, continue taking prescription medications as directed. If they are causing problems with potassium, work with your dietitian and doctor to come up with a plan to address the potassium issues as there are usually many causes of high potassium levels. Don’t have a dietitian? Learn more about our services here.
How eating too little sodium and potassium can make your potassium levels higher
Low sodium diets and or low potassium diets could actually be contributing to high potassium levels. When people find out that they have chronic kidney disease, they will often see on the internet or even hear from healthcare providers that they need to be following a low sodium and low potassium diet.
While it is true that many people would benefit from a lower sodium intake and some people may need to limit their potassium intake, some individuals can take it to the extreme and end up inadvertently causing problems with their potassium levels so let’s talk about how this happens.
Low sodium diets and hyperkalemia
The recommended sodium target for people with CKD is less than 2,300mg of sodium per day. Coincidentally, this is also the recommended sodium target for the general healthy population, so it really shouldn’t be called a low sodium diet because it’s the same as the general population.
However, a LOT of people consume way more than the recommended 2,300mg of sodium, so for those people, cutting down to 2,300mg may feel like a low sodium diet.
A key thing to understand with this target though is that the goal is not to go as low as possible. Unless you are end stage kidney failure with very little urine output or have some other condition requiring an ultra-low sodium diet, then I wouldn’t recommend going below 1,500mg of sodium. Eating too little sodium can affect the kidney’s ability to balance sodium and potassium levels.
There was an interesting case of a cardiologist who actually had chronic high potassium levels for 5 years. He also followed a VERY low sodium diet of somewhere between 500-1,000mg of sodium each day. He’s a cardiologist, and he sees every day the damage that a high sodium diet can cause, so that’s probably what motivated him to follow this super low sodium diet.
He didn’t have any risk factors for high potassium levels, and it took his doctors awhile to figure out that it was the low sodium diet that was causing it. When they had him increase his sodium intake, his hyperkalemia, or high potassium levels, went away.
He had high potassium levels for FIVE years and all it took was raising his sodium intake. When he ate only 500mg of sodium, which is an extremely low amount of sodium to eat, his potassium level was 5.8, which is pretty high. When he ate 1,000mg of sodium, it dropped to 4.8, which is now in the normal range. And when he ate 2000mg of sodium, it dropped down to 4.1, which is also normal.
If you are following a low sodium diet, the goal is not to eat as little sodium as possible. As you can see, eating too little sodium can also cause problems. I typically recommend that people with chronic kidney disease eat between 1,500 and 2,300mg of sodium each day unless otherwise instructed by your healthcare provider.
The recommended sodium intake is less than 2,300mg, but we don’t recommend less than 1,500mg of sodium unless instructed by your healthcare provider.
Low potassium intake and hyperkalemia
Similar to sodium, potassium restriction can ironically train your body to be worse at handling potassium.
Many people with CKD restrict their potassium intake when they don’t need to. They read it somewhere online that they should be watching their potassium intake, so they start to restrict potassium intake on their own, which can ironically just make things worse.
Most kidneys can remove sufficient potassium until they reach a GFR of <15. What that means is that if you eat too much potassium (within reason), your kidneys can usually remove it as long as there isn’t something else going on in your body that can cause it to get out of whack.
If you have a GFR of more than 15, then there is a really good chance that you don’t need to restrict potassium intake. If your potassium levels get too high and you have a GFR of more than 15, then it would be best to explore some of the other common causes of high potassium levels not related to food intake.
Do not restrict your potassium intake unless you have been explicitly told to do so by your healthcare provider, and even then, sometimes getting a second opinion from someone that specializes in kidney nutrition can be helpful because sometimes even healthcare providers can be a little too quick to jump to a potassium restriction too early in kidney disease.
Restricting potassium intake when you don’t need to will train your body to handle potassium less efficiently in a phenomenon called potassium adaptation.
When you eat high potassium foods, your body typically releases insulin, which helps your body balance out the glucose in your blood but it also helps balance out potassium by signaling to the cells of your body to remove some potassium from your blood. Researchers have found that the less potassium you eat, the less your body’s cells will respond to insulin and take up potassium.
If you are regularly eating a very low potassium diet, it’s almost as if you are training your body to leave the potassium in the blood because you don’t eat very much of it, and the body doesn’t want you to get low potassium levels.
This means that if you have been really limiting your potassium intake when you don’t need to be, you can inadvertently be making it harder for your body to control potassium.
Much like sodium, the goal with managing potassium levels is not to eat zero potassium. Your body still needs potassium to function properly. In my experience, a lot of people seem to focus on a target of 2,000mg of potassium or less – despite the fact that there is no official target potassium intake.
For a lot of people with CKD, 2,000mg is going to be too low and cause you to eat more foods that are not good for your kidneys.
Low potassium foods tend to be highly processed, high in sugar, and lacking in essential nutrients and fiber like the candy, white bread, cookies, and sugary cereal below.
While foods naturally higher in potassium like fruits and vegetables tend to have a lot of really beneficial nutrients.
Fruits and vegetables are going to be higher in fiber, which helps with constipation and can help remove potassium from the body.
Fruits and vegetables are going to help fight metabolic acidosis, which is going to help you control your potassium better. Fruits and vegetables are going to be higher in essential vitamins and nutrients.
On top of all of these benefits, we can see that by eating some potassium, we can keep our cells trained to help remove potassium from the blood when needed.
While you may not need to eat the 3,400 – 4,700mg of potassium that is recommended for the general population, you should not be overly focused on reducing your potassium intake as much as possible unless it has been determined that you truly need a potassium restriction (and even then, the goal is still not to be a low as possible).
Be sure to talk to your healthcare providers to determine the right goal for you.
How to include more fruits and vegetables while managing potassium levels
Including more fruits and vegetables in your diet is one of the best things that you can do for your kidneys. It is also one of the best things that you can do for managing or preventing other conditions as well such as diabetes, hypertension, gout, high cholesterol, heart disease, and cancer – eating more fruits and vegetables is beneficial for all of these conditions.
We are really starting to see more and more research showing that people who eat more fruits and vegetables have better outcomes when it comes to kidney disease, so we really want to make sure that we are eating enough fruits and vegetables.
However, fruits and vegetables do tend to be higher in potassium compared to some other foods, so let’s talk about some strategies for how to include them if you are concerned about adding too much potassium.
First off, fruits and vegetables can actually help your body be more efficient at handling potassium:
- One of the more common causes of high potassium levels is metabolic acidosis, and diets that are low in fruits and vegetables are more acidic. Eating more fruits and vegetables can help reduce the acidity and enable your body to control potassium levels better, which is just one of the benefits of controlling metabolic acidosis better.
- Another way that fruits and vegetables can help with controlling potassium levels is by increasing the amount of fiber in the diet. Fiber helps prevent constipation, and we know that constipation – especially in people with kidney disease – can cause high potassium levels because the body isn’t able to use bowel movements to remove extra potassium from the blood. Fiber also helps with blood sugar control, so that’s a win win if you have diabetes as well.
- Vegetables also stimulate some insulin release, so your body will be able to handle some extra potassium in the food by storing the extra inside your cells. 200mg of potassium from a fruit or vegetable is going to be handled much better by your body than 200mg of potassium added to a sports drink.
This means that eating more fruits and vegetables, which are arguably higher in potassium than many other foods, is not necessarily going to raise your potassium levels because of all of these ways that they help your body control potassium.
Additionally, there are so many benefits to fruits and vegetables for kidney disease and other chronic diseases that we really want to be sure that we are eating enough fruits and vegetables.
The Dietary Guidelines for Americans recommend that adults should aim for 1.5-2.5 cups of fruits per day and 2-4 cups of vegetables per day, which is something that people with CKD should strive for as well.
If you are concerned about your potassium levels or if you’ve been told that you need to cut back on how much potassium you are eating, it can be a bit daunting to start including more fruits and vegetables into your day.
High fiber, Low Potassium Fruits and Vegetables for CKD
One good strategy is to focus on getting in higher fiber fruits and vegetables first. Focusing on adding the higher fiber fruits and vegetables first will help alleviate constipation, which will in turn help improve how much potassium your body is able to remove.
Start by focusing on higher fiber, lower potassium fruits and vegetables. Most kidney professionals consider a fruit or vegetable to be low in potassium if it contains less than 200mg of potassium per serving, so searching for those lower potassium fruits and vegetables is a good starting point.
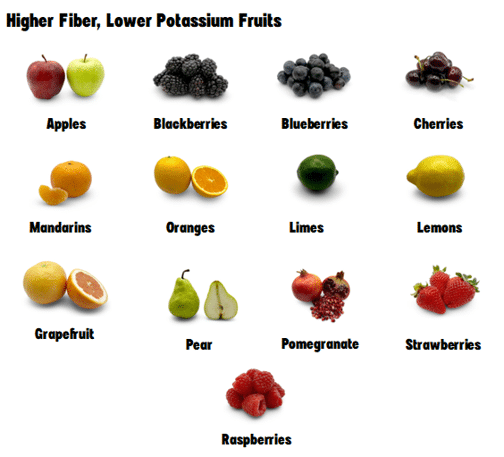
For fruits, these are some of the higher fiber, lower potassium fruits. If you are trying to watch your potassium intake, then definitely gravitate towards higher fiber choices.
And if you have diabetes, keep in mind that fruits do tend to be higher in carbohydrates, which means we do need to be mindful of the overall carbohydrate content of meals and snacks. Focusing on fruits that have a higher fiber content can also really help with reducing the blood sugar spikes since fiber helps slow down digestion. We also recommend pairing fruit with something high in fat, such as nuts, to further help slow digestion.
You might be surprised to see oranges on that list of lower potassium fruits. Oranges get a bad rap for being high in potassium, but that is usually related to orange juice.
One orange, which is actually considered two servings of fruit – we’ll talk about serving sizes in just a moment – , has 238mg of potassium, so half an orange which would be one serving has only 119mg of potassium, which is pretty low.
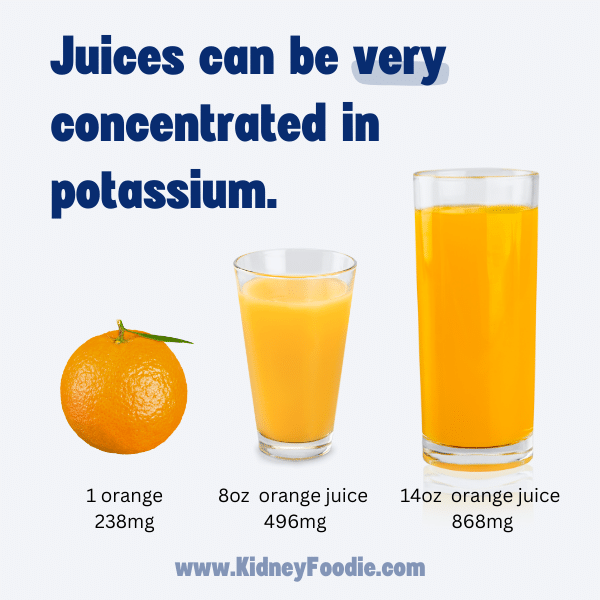
In contrast, if you were to drink an 8oz cup of orange juice, you would be getting almost 500mg of potassium. And Orange juice is really easy to over-consume. A typical drinking glass can usually hold 12-14 ounce of juice, so if you were to drink a whole glass of orange juice, now you’re up to almost 900mg of potassium – and zero fiber! So, oranges are definitely okay to enjoy, but orange juice can get out of control pretty fast.
For vegetables, here are some low potassium vegetables you can try.
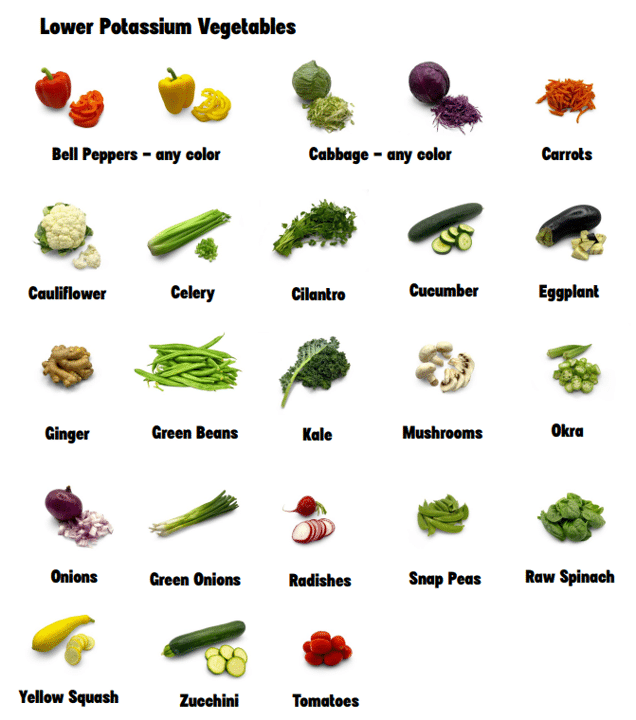
One thing I want to point out about vegetables is that some vegetables shrink a lot when cooked, so the raw version may be considered low potassium, while the cooked version would be considered high potassium.
A good example of that is spinach. One cup of raw spinach has only 146 mg of potassium while ½ cup of cooked spinach contains 486mg of potassium. Spinach shrinks A LOT when cooking and it takes almost 3.5 cups of raw spinach to make ½ cup of cooked.
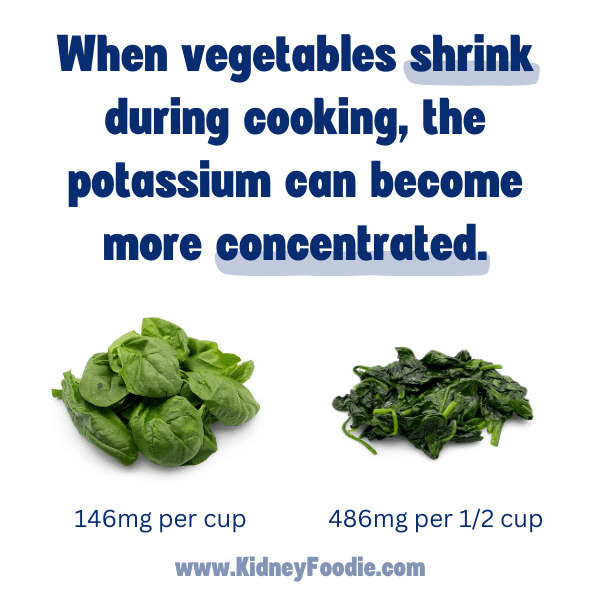
Be sure to keep that in mind how vegetables might shrink during cooking and become more concentrated in potassium. If you don’t have a potassium restriction, then this doesn’t matter as much (and cooked spinach will have a lot of acid neutralizing compounds, antioxidants, etc, so still good for you), but if you are watching your potassium intake, this would be something to keep in mind.
If you don’t want to hold onto a list of low potassium fruits and vegetables, I recommend bookmarking our fruit and vegetable tool on your phone or computer.
Fruit and Vegetable Serving Sizes and Potassium
One thing to keep in mind with fruits and vegetables and potassium is that serving size matters. The more of a certain food that you eat, the more potassium it will have.
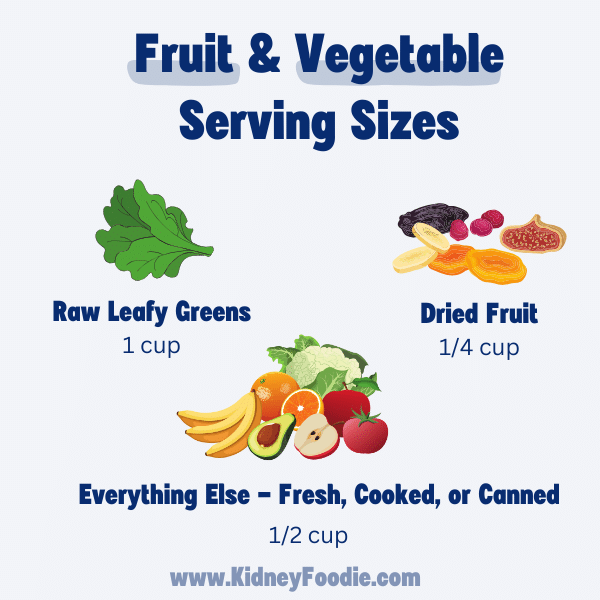
For the majority of fruits and vegetables, the serving size is ½ cup.
One of the main fruits I like to point out when I talk about serving size is watermelon. Watermelon is technically a low potassium fruit – IF YOU ONLY EAT HALF A CUP. One 60g half cup of watermelon has roughly 67mg of potassium. If you eat a whole watermelon, that’s over 5,000mg of potassium. Not to mention that’s a lot of sugar!
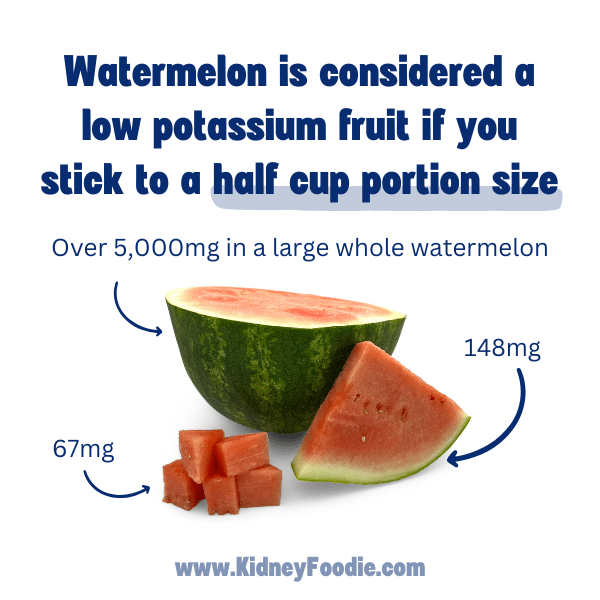
If you need to be mindful of potassium, then be mindful of portion sizes.
There are two exceptions to the ½ cup serving. The first exception is raw leafy greens, like spinach. The serving size of raw leafy greens is 1 cup. The other exception is dried fruit. The serving size of dried fruit is typically only one ounce which roughly ¼ cup.
Limit juices and dried fruits to avoid too much potassium
When adding more fruits and vegetables to your diet, I strongly recommend that you select fruits and vegetables that are as minimally processed as possible. Juice and dried fruits are examples of processed fruits that can be problematic for people with problems controlling their potassium levels.
A serving of juice is almost always going to be higher in potassium than the equivalent amount of fruit, which we demonstrated with the orange juice example earlier in this page.
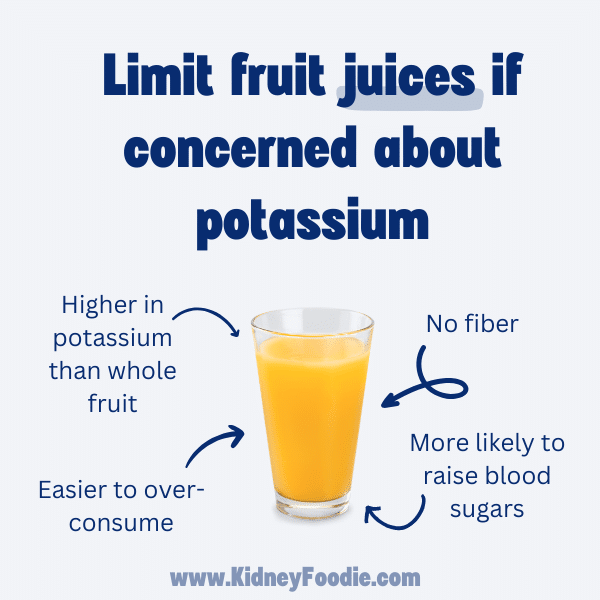
Juice is really easy to over-consume. Juices are also typically VERY high in sugar, so if you have diabetes juice will spike your blood sugar. Juices also don’t have any fiber, which means they do not help prevent constipation.
Eating the whole fruit instead of juice will limit the overall portion size PLUS it will have fiber that helps slow down the digestion of some of the sugar and help improve your body’s ability to manage potassium through your bowel movements.
If you really like to drink your fruit, smoothies may be a better option. With smoothies, you blend the whole fruit, so you will still get the benefits of the fiber in the drink.
Dried fruits are also a concern. While dried fruits still contain some fiber, they will be very concentrated in potassium. Many dried fruits also contain added sugar and many will also contain potassium additives, which further drive up the potassium content.
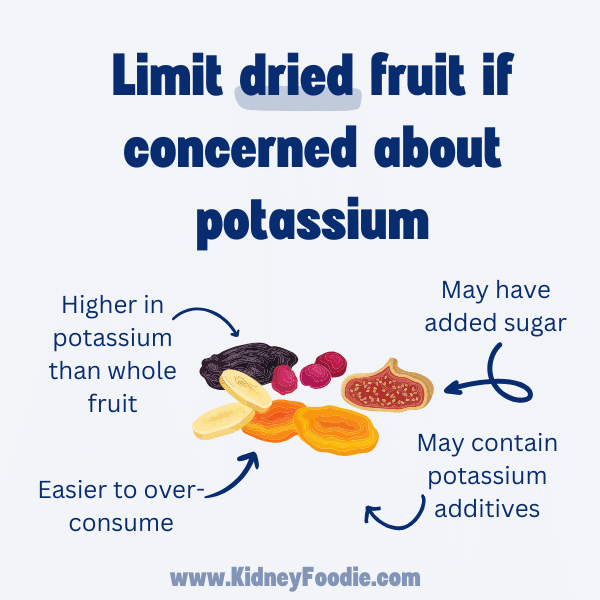
If you choose to eat dried fruit, be sure to keep the portion size of one ounce or ¼ cup in mind and select fruit that does not contain added sugar or potassium additives.
Including High Potassium Fruits and Vegetables in the CKD Diet
If you have been told to reduce your potassium intake, it does not mean that you can never have a high potassium fruit or vegetable ever again. As an example, I just want to show you a sample meal plan from our CKD course just to show you that you CAN include higher potassium foods and still end up with a lower potassium day.
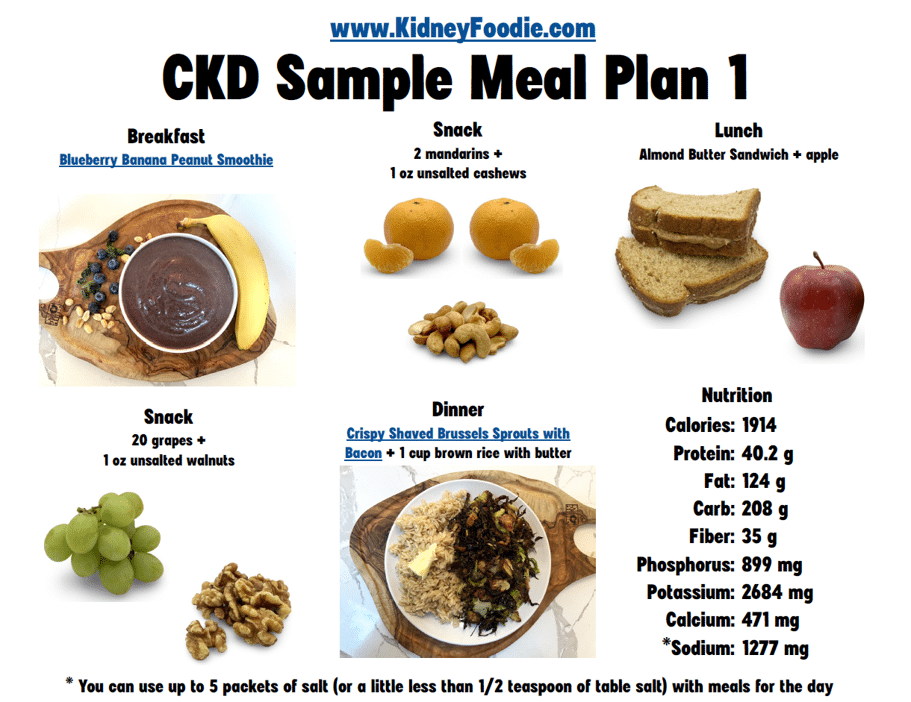
This menu has 1,914 calories and only 2,684mg of potassium – which is pretty low. For healthy adults with no kidney problems, it is typically recommended to eat 4,700mg of potassium, so this menu has 2,000mg less than that.
What you may or may not notice about this menu though is that it contains more than 6 cups of fruits and vegetables and as part of those fruits and vegetables, I’ve included banana, which is frequently considered too high in potassium to include as well as a pretty hefty serving of brussels sprouts, which are considered high potassium vegetables.
My point with showing you this meal plan is to emphasize that you do NOT have to give up your favorite fruits and vegetables if you don’t want to. We can find ways to include higher potassium fruits and vegetables if that is what you want.
Also, if you are nervous about the idea of including more fruits and vegetables or including a higher potassium fruit and vegetable into your diet, then I would consider doing a little experiment before your next labs. The night before your next labs, I want you to choose a higher potassium fruit or vegetable to eat and see if your labs are actually all that different. This way, you can get that quick feedback on whether or not your body can tolerate a little more potassium. There is a good chance that it can – especially if you’ve been working on fixing some of the other common causes of high potassium like constipation or metabolic acidosis and such.
How food preparation methods affect the potassium content of foods
The way that a food is processed or prepared can significantly affect the amount of potassium that is in it. If you need to limit your potassium or you are trying to be more mindful of your potassium intake, then understanding how processing and cooking affect some foods can be really helpful.
One thing to understand about potassium is that potassium loves water. When you cook foods in water, potassium will actually leave the foods so that it can spread out into the cooking water.
One example of this is with canned fruits and vegetables. Canned fruits and vegetables tend to be precooked in liquid, which helps remove some potassium. Then they are canned in liquid, which further allows potassium to diffuse out of the fruits or vegetables.
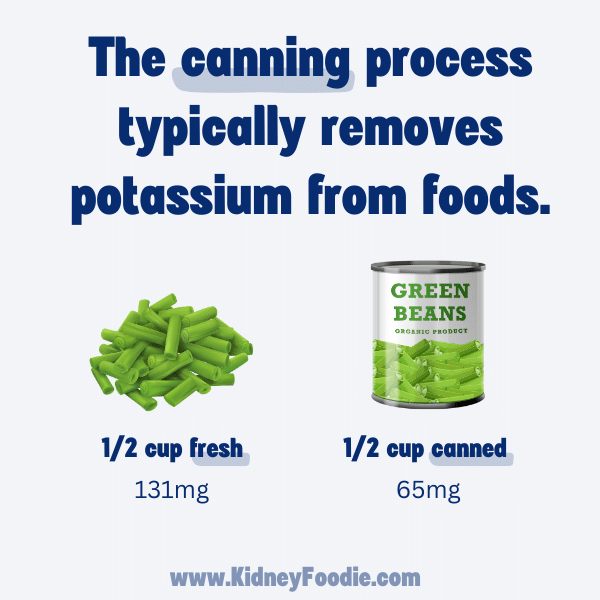
This means that canned vegetables will be lower in potassium than their fresh counterparts. For example, one half cup (~62g) of fresh green beans contains 131mg of potassium while one half cup of canned green beans contains only 65mg of potassium.
The same principle applies to other canned goods like beans. For example, ½ cup of boiled chickpeas (about 82g) contains ~240mg of potassium while ½ cup (or 76g) of canned chickpeas that have been drained of the liquid and rinsed with fresh water will contain only 83mg of potassium. So canned foods can be a good option for people who are trying to watch their potassium intake.
Just be sure to choose canned foods with no salt added. Canned foods are notoriously high in sodium, so if you choose canned versions of fruits and vegetables, check the label to verify that there is no salt added. And if you’re selecting canned fruits, be sure to choose fruits that are packed in juice and not syrup. Syrup is just code for lots and lots of sugar, which we do not want.
When using canned foods, always drain the juice or liquid off before eating. The juice and liquid will contain a fair amount of potassium that has diffused out of the fruits and vegetables. Draining that liquid off will help reduce the potassium content of the food.

Additionally, rinsing the food in some fresh water can remove even more potassium.
Double boiling to remove potassium
You can also choose to double boil foods to remove excess potassium. This is most commonly recommended with potatoes, since potatoes are very high in potassium.
The general idea is the cut your potatoes and place them in a pot of water. You should use twice as much water as potatoes.
Bring the pot of water and potatoes to a boil, then drain and rinse the potatoes. Place them back in the pot and fill with twice as much fresh water, then boil again until the desired tenderness, and drain off the liquid and rinse the potatoes. If you do this, you can reduce the amount of potassium in your potatoes by about 40%.
A few key points to keep in mind when double boiling your potatoes is that the smaller the potato pieces, the more potassium will be removed.
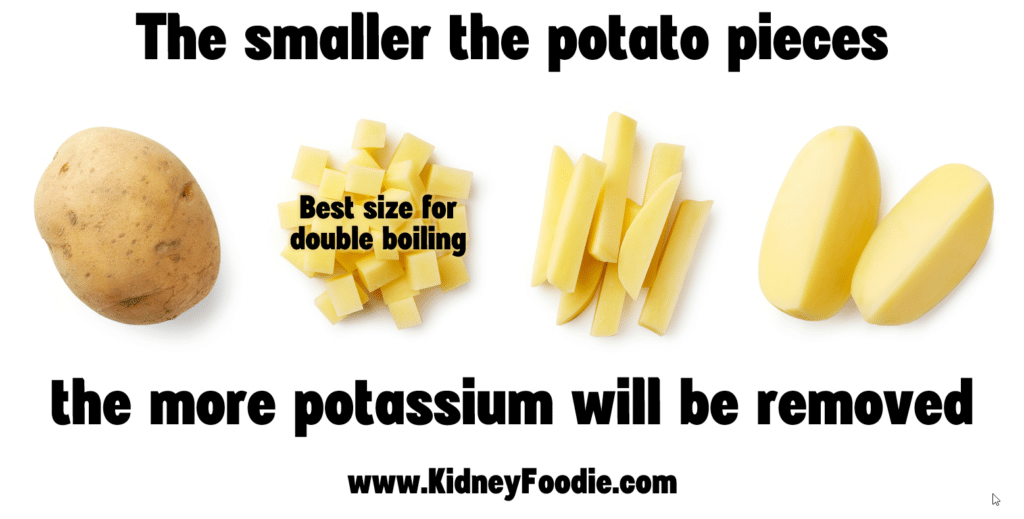
Boiling whole potatoes is not going to leach as much potassium out as using the diced potatoes. So be sure to cut them up pretty small to get the most potassium out. [CLICK] Second, I want to emphasize that you need to use enough water. The more water you use, the more potassium will be removed. Use twice as much water as potatoes. If you don’t use enough water, it won’t remove as much potassium. And you must be sure to change out the water when you boil the second time.
Lastly, for the folks who also have diabetes, double boiling potatoes doesn’t make them any more friendly for a diabetes diet. They are still going to be considered a starchy vegetable, which means they will raise your blood sugar. We still want to focus more on including more non-starchy vegetables.
However, double boiling is an option to lower the potassium of foods. You can do this with a lot of different vegetables, not just potatoes. The same method will apply.
Buying canned foods or double boiling foods can really help to lower the potassium content of foods. However, you do not need to necessarily do these things if you don’t have issues with potassium.
Most people with CKD do not have issues with their potassium, and we don’t need to be avoiding potassium if we don’t have to. Additionally, boiling and canning can remove other vitamins and nutrients as well, so we certainly don’t want to be losing out on other essential nutrients if we don’t need to limit potassium intake.
That being said, canned foods are convenient and maybe you actually enjoy double boiled food, in which case, feel free to enjoy.
Work with a dietitian
If you are having issues with potassium, I highly recommend working with a registered dietitian that is trained in working with kidney disease. Most insurance companies (including Medicare!) cover the cost of seeing a dietitian for Chronic Kidney Disease. To work with me, please click here.


